Numerous factors can contribute to kidney failure, a potentially life-threatening condition for your pet. The kidneys are critical for numerous important bodily functions, including waste removal, water conservation, red blood cell production, electrolyte and mineral balance, blood pressure regulation, and protein preservation. The Livingston Veterinary Hospital team knows that healthy kidneys are important for your pet’s overall wellbeing, so we provide information about what causes kidney failure in pets, and steps you can take to reduce your four-legged friend’s risk.
Acute kidney failure in pets
Acute kidney failure (AKF) is caused by a sudden injury to the kidneys that means they cannot function properly. Important AKF information includes:
- Causes — The most common AKF causes include insufficient blood supply (i.e., ischemia) to the kidneys, toxins, heart failure, burns, liver failure, cancer, kidney infection, urinary tract obstruction, hyperthermia, and sepsis. Pet toxins that can cause AKF include non-steroidal anti-inflammatories (NSAIDs), ethylene glycol, vitamin D2, and cardiac medications. Grapes, raisins, and currants are also kidney toxic for dogs, and lilies are kidney toxic for cats.
- Signs — AKF signs vary depending on the cause and disease severity. Potential signs include sudden onset and rapid progression of lethargy, inappetence, vomiting, diarrhea, and seizures. Pets’ thirst and urination may increase initially, but they may be unable to urinate when their condition worsens.
- Diagnosis — The following tests are typically performed when diagnosing AKF:
- Complete blood count (CBC) — A CBC evaluates your pet’s white blood cells, red blood cells, and platelets to help determine if infection or anemia is contributing to the problem.
- Biochemistry profile — Kidney biomarkers, including creatinine and blood urea nitrogen (BUN), which are evaluated on a biochemistry profile, are typically extremely elevated in AKF.
- Symmetric dimethylarginine (SDMA) — SDMA, another kidney biomarker that is more sensitive than creatinine and BUN, is also commonly tested when kidney failure is suspected.
- Urinalysis — A urinalysis evaluates the kidneys’ ability to concentrate urine, providing valuable information about kidney health.
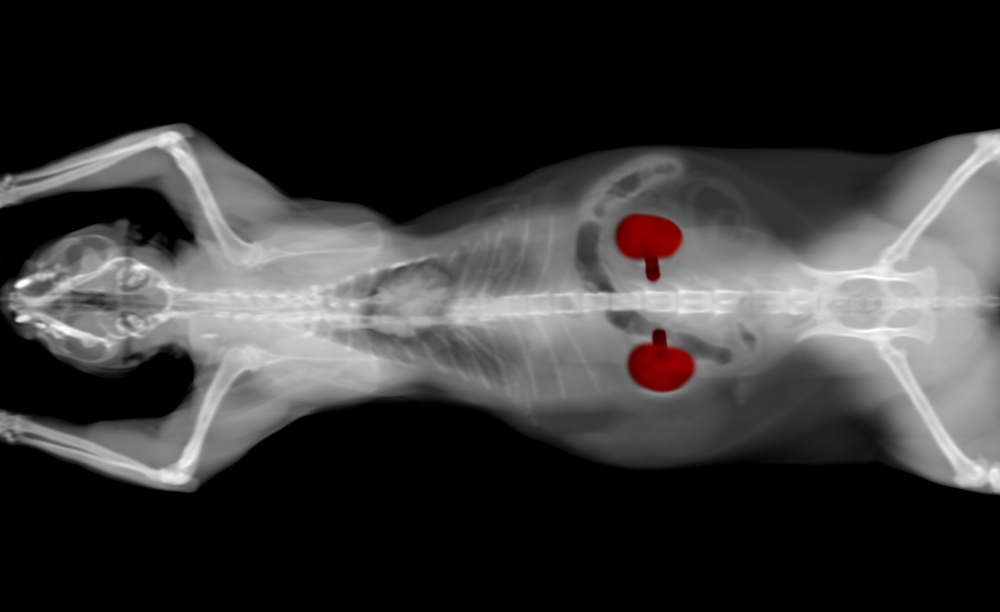
- Imaging — X-rays and ultrasound may be used to evaluate your pet’s kidneys.
- Treatment — AKF treatment involves intense intravenous fluid therapy to correct fluid loss, electrolyte imbalances, and acid-base disturbances, and medications to promote urine production. In toxicity cases, steps are taken to counteract the toxin. Prolonged hospitalization is typically needed to effectively treat AKF.
- Prognosis — When treated early, pets in AKF can survive, but many develop chronic kidney failure (CKF).
Chronic kidney failure in pets
CKF is common in pets, especially older pets, and slowly inhibits kidney function over months or years. Important CKF information includes:
- Causes — Pets affected by AKF can develop CKF, although the inciting cause is usually unknown.
- Signs — Affected pets typically don’t show signs in the initial stages, but then exhibit lethargy, decreased appetite, bad breath, increased thirst and urination, weight loss, and vomiting as the condition progresses.
- Diagnosis — The same tests used to diagnose AKF are used for CKF. In addition, CKF pets are staged to help determine an appropriate treatment strategy. CKF staging includes:
- Stage I — Clinical signs are absent, but SDMA levels are slightly elevated, and other laboratory values are usually normal.
- Stage II — Clinical signs are mild or absent, and laboratory values, including SDMA, creatinine, and BUN, are mildly elevated.
- Stage III — Clinical signs are mild or moderate, and laboratory values, including SDMA, creatinine, and BUN, are moderately elevated.
- Stage IV — Clinical signs are evident, and laboratory values, including SDMA, creatinine, and BUN, are significantly elevated. These pets are at high risk for a medical crisis.
- Treatment — Our team will devise a specific treatment protocol based on your pet’s condition and staging. Treatment regimens typically include:
- Fluids — Maintaining your pet’s hydration is paramount, and we may recommend administering subcutaneous or intravenous fluids.
- Renal diet — Prescription renal diets are low in protein, phosphorus, and sodium, and high in water-soluble vitamins, fiber, and antioxidants.
- Anti-nausea medications — Since CKF can cause vomiting, we may prescribe anti-nausea medications.
- Phosphorus binders — Phosphorus levels are commonly elevated in CKF, and we may recommend phosphorus binders to combat this problem.
- Erythropoietin — If your pet experiences anemia associated with CKF, they may need erythropoietin injections.
- Prognosis — Pets with CKF can’t be cured, but they can live a relatively normal life with early detection and long-term management.
Preventing kidney failure in pets

Not every kidney failure case can be prevented, but steps you can take to reduce your pet’s risk include:
- Scheduling regular wellness exams — Regular wellness visits allow us to detect conditions such as CKF in the early stages, when they are easier to treat and have a better prognosis.
- Brushing your pet’s teeth — Periodontal bacteria can enter your pet’s bloodstream and damage their kidneys. Brushing your pet’s teeth daily keeps their mouth and kidneys healthy.
- Avoiding toxins — Educate yourself on what substances are toxic to pets, and take steps to ensure your pet is not exposed.
Contact our Livingston Veterinary Hospital team to schedule your pet’s annual wellness exam, so we can ensure their kidneys are in tip top shape.






Leave A Comment